A small clinical trial used immunotherapy that surprisingly shrank the tumors of young adults and children who were diagnosed with rapidly growing diffuse midline gliomas (DMGs) known as H3K27M mutant. The mutant has been identified in almost 80% of young patients with the disease.
As reported by the NIH, this form of spinal cord cancer and brain cancer affects young adults and children. It spreads into surrounding areas and has an overall survival rate of eleven to sixteen months.
A team of Stanford University researchers created a CAR-T therapy that targets GD2 which is a molecule made in vast quantities by H3K27M. Ongoing trial results were published in 2024 in the journal Nature.
Stanford Medicine’s Dr. Crystal Mackall described the improvements as “contrary to general belief”, CAR-T cells appear promising in treating solid tumors, especially tumors that express the GD2 antigen solid cancers.
Nine out of eleven patients receiving the GD2 CAR-T exhibited neurological improvement. It is noted that as the tumors shrank, the patients’ symptoms improved with many patients regaining the physical mobility lost due to the disease.
Participants in the trial lived on average, almost two years after receiving treatment. Two participants are still alive after 2.5-years with one patient experiencing a disappearance of the tumor and is still free of his cancer four years after initial diagnosis.
Dr. Rosandra Kaplan at the NCI Center commented that nothing has been effective thus far and believes that the trial will vastly improve treatment methods.
Certain cancers present a challenge in surgical removal, however, due to their location in the brain controlling vital functions.
Radiation and chemotherapy only provide temporary relief while patients almost immediately lose many critical functions.
What is CAR T-cell Therapy (CAR-T)
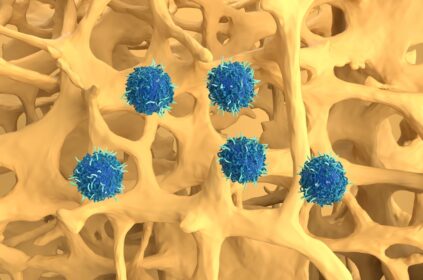
CAR-T immune cells are extracted from the patients’ blood. The cells are genetically modified to express CAR-T then reinfused into the patients’ blood stream. The CAR-T cells seek cancer cells and upon recognition begin an immune response that destroys them.
The approach is challenging, as the molecules that are being targeted are not only on the surface of the tumor but are also on healthy cells.
About GD2
Dr. Mackall developed a CAR-T therapy that targets GD2 and began testing. GD2 was found in the tumors of patients with osteosarcoma and neuroblastoma. Using a mouse model, the teams demonstrated that GD2 CAR-T therapy penetrates the brain and destroy tumors.
Eleven young adults and children with either spinal DMG or DIPG received an intravenous infusion directly into the brain of one or two doses of CAR-T or GD2. The team observed that there was less inflammation resulting from the lower dose.
Nine patients experienced satisfactory results after receiving their first treatment. These patients continued GD2 CAR-T infusions every one to three months if the disease continued to be stable.
Adverse reactions to the treatment were primarily neurological issues such as fluid buildup, headaches, and fever, all issues that are often seen in inflammation of the spinal cord and brainstem and can be managed by using standard approaches.
Presently the Stanford Clinical trial is operational, with patient groups receiving treatments directly into the brain.
Dr. Kaplan and her team are conducting their own clinical trial using the same CAR-T treatment for patients who have been diagnosed with osteosarcoma and neuroblastoma that express GD2 at high levels.
A larger phase 2 trial is being prepared by Dr. Mackall’s team enrolling not only Stanford patients but patients from several other centers.
Editor’s Note: Get Involved
Cancer doesn’t discriminate. WHATNEXT and its partners are interested in amplifying the voices of those from all identities and backgrounds. If you have a cancer journey to share, reach out here to learn more about how your voice can help spread awareness and inspire individuals from all walks of life.
CAR-T CAR-T cell therapy NIH Pediatric Brain Cancer Pediatric Spinal Cord Cancer
Last modified: April 7, 2025